Links to the CHAPTERS: [ HOME-Page ] [ FACTS & INFORMATION ] [ RECOGNIZE & TREAT]
Chronic inflammation of the eyelids (chronic blepharitis), mainly of the eyelid margin with the eyelashes, is often associated with other disease conditions of the ocular surface such as chronic dry eyes and Meibomian gland dysfunction (MGD).
Blepharitis & Bugs: Bacterial infections or excessive growth of normal bacteria and of the normal Demodex hair mites can often occur.
Therapy: Eyelid hygiene and lidcare is a foundation of blepharitis therapy. Excessive Demodex infestation may need a specific therapy, if diagnosed by an eye doctor.
=> here is a short general overview of eyelid therapy options.
On this page you will find the following topics:
Chronic blepharitis is typically a long standing condition with red and slightly swollen eyelid margins which often cause few complaints. - It is important to exclude other more acute and more severe conditions - therefore an eye doctor should always be consulted !
Chronic inflammatory reactions of the eyelids (chronic blepharitis), particularly of the lid margin, often occur in dry eye disease and in Meibomian gland disorders.
In theory there are two different types of blepharitis:
An anterior type of blepharitis is located at anterior lid border at the eyelashes and is influenced by bacteria or Demodex hair mites. Here the inflammation is typically clinically visible and recognizable by redness and thickening of the lid margin - this forms the typical picture of "chronic blepharitis" (please see image). Bacteria play a role but it is not always an "infection" but more often an overgrowth of normal commensal bacteria. This is favored by a disturbed environment on the eyelid margin and on the eyelashes.
The posterior type primarily affects the posterior lid border with the meibomian glands (please see image). In this case, the inflammation is typically subclinical, which means that there are inflammatory mediators and an inflammatory response in the tissues, but this is not clinically obvious. Meibomian gland dysfunction (MGD) is the main form of posterior blepharitis. Because MDD is very common, it is, simply put, virtually identical to posterior blepharitis.
However, both forms of eyelid inflammation often overlap and cannot always be clearly separated. A chronic eyelid inflammation is typically recognized by the reddened and swollen eyelid margin (please see image).
Chronic inflammatory skin disease, such as atopic dermatitis (neurodermatitis), rosacea or seborrheic dermatitis (seborrheic eczema) can induce or favor a chronic blepharitis.
Chronic blepharitis does not necessarily present with bothersome, irritating symptoms. If it develops very slowly with advancing age and is associated with minor eyelid changes, it may occasionally go unnoticed by the patient.
Therapy options:
Eyelid hygiene for a targeted cleaning of the eyelids from inflammation-promoting depositions with subsequent eyelid care, is an important first therapeutic measure.
If a dry eye is also present, tear supplements or other options of the staggered dry eye therapy can often also contribute to improvement a co-existing blepharitis.
Further steps could be prescription medicine against inflammation or against an infection, if this is present. Some medications combine both functions, if necessary.
If there is an underlying disease, such as e.g. a chronic skin disease that may also affect the eyelids, a therapy of the underlying disease is of course important.
Overall, it is important to see your ophthalmologist, who can determine which disorder is present and recommend an appropriate therapy !
Chronic inflammatory skin disease is a risk factor
Chronic inflammatory skin disease can trigger or promote chronic blepharitis and is thus a risk factor.
Atopic dermatitis usually shows dry, rough, scaly skin, which can also be wet and is usually very itchy. The disease can affect the entire body including the face and eye area. It often occurs in phases and leads to a thinning of the skin with increased wrinkling.
Rosacea (Akne rosacea) is a chronic inflammation of the face, especially the cheeks, nose and eyes and the upper part of the body (décolleté). Dilatation of the blood vessels causes the redness of the affected regions, which leads to the name rosacea. Increased activity of the sebaceous glands, with oily skin, and of the connective tissue leads to an overall thickening of the skin.
Seborrheic dermatitis (seborrheic eczema) is a chronic inflammatory skin rash with scaling and hyperactivity of the sebaceous glands. Infestation with yeast fungi and possibly bacteria on the damaged skin areas can play a role. In addition to the chest and back, the disease occurs mainly on the head and face and can also lead to chronic inflammation of the eyelids (chron. blepharitis). It leads to oily skin and with the formation of yellowish oily crusts.
Deposits and incrustations on the lid margin favor DEMODEX mite infestation
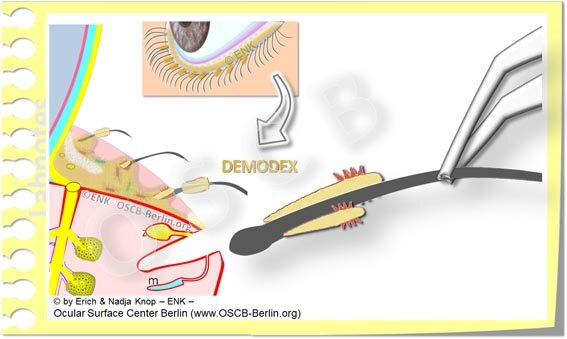
The harmless normal Demodex Hair Miltes reside in the hair follicles of the eyelashes, where they also multiply. They are mobile and can glide along the lashes. Their remains form typical cylindrical scales at the base of the eyelashes. In case of chronic eyelid inflammation (chronic blepharitis) the number of demodex is increased.=> here is a microscope image of Demodex mites
Deposits and incrustations on the lid margin and at the eyelashes occur in all chronic forms of the dry eyes, in Meibomian gland dysfunction and in blepharitis. They can be important disease-promoting factors.
The deposits are related to excessive growth of normal lid margin bacteria and of the normal and basically harmless Demodex hair mites at the eyelashes. Demodex and bacteria contribute to the accumulation of such depositions
The depositions of debris on the lid margin contain skin-irritating substances and can thus lead to an worsening of the eyelid inflammation.
Demodex hair mites can be detected at the slit lamp by the ophthalmologist.
=> here is a short general overview of therapy options for the eyelids and dry eyes
=> here are therapy options for Demodex hair mites
Demodex Mites on a glass object tray as seen in a light microscope (upper image) - they live in the hair follicles of the eyelashes. Their remains often form typical cylindric deposits at the base of the eyelashes (lower image). Images courtesy of Laboratoires Théa.
The small Demodex hair mites are almost invisible to the nakes eye because their size is only about 0,5 Millimeter.
Furthermore, they hide in the hair follicle of the cilia and thus reside ´under cover´ ;-)
But Demodex mites reveal themselves by changes on the edge of the eyelid and the eyelashes:
In overshooting Demodex infestation, the eyelid margin is usually covered with solid or liquid-oily deposits. This is probably not caused by demodex alone but indicates that the mites find nutrients here and feel "well".
At the base of the eyelashes are cylindrical yellowish deposits. These are remains of Demodex mites, which are deposited here and form collar-like deposits around the base of the lashes. These so-called 'collarets' are visible on closer examination (please see image).
Suspected diagnosis: Demodex … If
a chronic eyelid inflammation (blepharitis) occurs
with deposits on the eyelid margin and at the base of the lashes
which does not improve significantly despite regular daily eyelid cleaning and care
… then Demodex skin mite infestation can usually be detected relatively easy by the ophthalmologist at the slit lamp.
Demodex hair mites can often be seen better in the slit lamp if the eyelashes are twisted against the direction of growth using tweezers
The normal Demodex hair mites at the eyelashes seem to play a role in blepharitis and dry eye, as their number was found to increase with the severity of the disease.
So far it is not entirely clear whether Demodex mites are a triggering factor of blepharitis or whether they only multiply strongly with an increase of nutrients in the disturbed environment.
Demodex become visible in the hair funnel
when small tweezers are used to bend individual eyelashes against the direction of growth.
a number of eyelashes can be inspected in this way at the slit lamp
to determine the amount of the demodex infestation.
After removing an eyelash, Demodex mites typically hang from the hair follicle and can be diagnosed on the slit lamp.
Alternatively, single eyelashes can be plucked out, which is painless,
it is then relatively easy to see the small mites in a larger magnification at the slit lamp
If Demodex only occurs at few individual eyelashes, this is regarded as normal and usually harmless
However, if Demodex is found on a majority of eyelashes and in larger numbers, this is an indication of an increased infestation.
This should be treated with means that effectively eliminate Demodex. Tea tree oil active ingredients are currently considered the most effective therapy.
Therapy-resistant blepharitis - watch out for Demodex
In cases where conventional dry eye therapy for Meibomian gland disorders and chronic blepharitis remains without significant improvement, it may make sense to carry out specific therapy to reduce Demodex mites.
Therapy options against DEMODEX mites:
Tea tree oil and its active ingredients have proven their worth here.
Natural tea tree oil, that is available in big bottles, has a strong irritant effect. Therefore extracts of the specific active ingredient in tea tree oil against Demodex have now been developed, which are better tolerated.
Tea tree oil or its main active ingredient is offered ready prepared:
on cleaning cloths with which the eyelid margin and eyelashes can be cleaned directly
as a foam, which contains tea tree oil extracts in different dosages and allows a thorough cleaning of the eyelid margin.
Tea tree oil is used in the form of a cure in which the cleaning is repeated daily until the symptoms improve.
Therapy options of Demodex mites based on tea tree oil active ingredients
... for chronic blepharitis with excessive infestation with Demodex skin mites
Demodex hair mites are resistant to common antiseptics and therefore cannot be eliminated by simple eyelid cleaning.
Tea tree oil is effective against demodex hair mites on the eyelids However, it typically causes severe irritation of the skin and eye and may also cause allergies. The main ingredient is terpinen-4-ol, which is also the main active ingredient against Demodex. It is better tolerable and causes less irritation compared to complete tea tree oil with its numerous components. Tea tree oil and also terpinen-4-ol can kill demodex mites with different efficiency.
However, tea tree oil or terpinen-4-ol alone does not completely eradicate Demodex mites, but only if an additional scrubbing eyelid cleansing is performed to mechanically remove the mites from the hair follicles of the eyelashes - as is typically done with cleansing wipes. It may be useful to leave the active ingredient on for a few minutes and not wash it off with water immediately, as the killing effect takes some time.
In case of strong deposits of incrusted oils and debris on the eyelid margin with distinct signs of inflammation (redness, swelling), even without significant infestation with Demodex hair mites, it may be useful to make a therapy attempt with tea tree oil cleansing wipes, since tea tree oil and its active ingredients, according to studies, have many useful effects, e.g. antibacterial anti-fungal, anti-inflammatory.